Today’s post is about a drug originally proposed by Wayne State University in the US, but so far approved and widely used mostly in Asia. China is the big producer/user and Italy is the outlier where it is also used.
Therapeutic Developed in United States Benefits Many in Asia
Since Wayne State University gastroenterologist Milton Mutchnick, M.D., first proposed using the hormone-like peptide thymosin alpha 1 to combat Hepatitis B in the mid-1980s, the drug has seen both outstanding success and somber letdown. Overseas, thymosin has become an important tool for fighting Hepatitis B, cancers and infections. Within the United States, its promise remains in doubt decades later.
Today we consider
repurposing a naturally occurring peptide from the thymus to restore
balance/homeostasis to the immune system in people with autism.
It has been
well documented in the research (for example by Paul Ashwood at the MIND
Institute) that the immune system can be dysfunctional in many people with
autism, but in different ways.
Some people
with autism suffer from flare-ups when their symptoms get much worse. These flare-ups can be immune mediated,
meaning that the rather complicated pro-inflammatory / anti-inflammatory
balance has been disrupted. A reset is
needed.
In some
cases, a short course of oral steroids is enough to provide the reset, but
often it does not work.
One reader
of this blog was proposed by his Italian doctor to try Thymosin alpha 1 shots to treat
his son’s autism flare up. Not
surprisingly, living in the UK, he had never heard of Thymosin alpha.
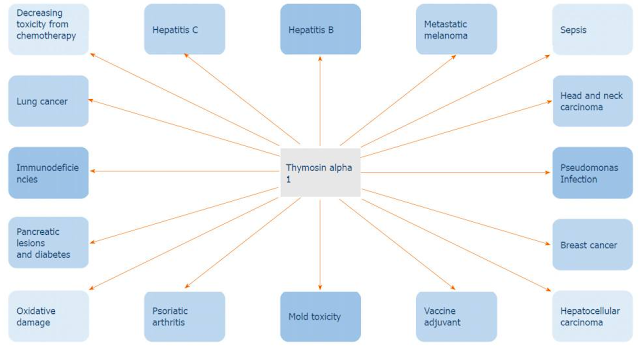
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7747025/figure/F2/
What
is Thymosin alpha 1?
The following paper
provide an excellent explanation:
Thymosin alpha 1: A comprehensive review of the literature
Thymosin alpha 1 is a peptide naturally occurring
in the thymus that has long been recognized for modifying, enhancing, and
restoring immune function. Thymosin alpha 1 has been utilized in the treatment
of immunocompromised states and malignancies, as an enhancer of vaccine
response, and as a means of curbing morbidity and mortality in sepsis and
numerous infections.
Thymosin alpha 1 has long been recognized as an
immune enhancing, immune modulating, as well as an immune restoring agent, and
as such it has been utilized in several clinical and research settings. The
synthetic form of thymosin alpha 1, thymalfasin, is approved in more than 35
countries for the treatment of hepatitis B and C and as an immune enhancer in
several other diseases
Thymosin alpha 1
functions as a toll-like receptor (TLR)-9 and TLR-2 agonist in both myeloid and
dendritic cells, the professional antigen-presenting cells. By targeting TLRs,
thymosin alpha 1 can stimulate the adaptive immune response, which is essential
for fighting viral, bacterial, and fungal infections and cancers, as well as
stimulation of posterior humoral immunity. Additionally, thymosin alpha 1 can
increase levels of IL-2, IL-10, IL-12, interferon (IFN)-α, and IFN-γ. The role
of thymosin alpha 1 in stimulating T-cell dependent antibody production is also
the reason why it has been considered as a vaccine adjuvant for enhancing
response to vaccines.
Thymosin alpha 1 has a wide range of biological
activities that range from anti-tumor to immune-modulating properties. The
immune response of thymosin alpha 1 is due to its action in elevating the
activity of T cell maturation into CD4+/CD8+ T cells. It works to directly
activate natural killer cells as well as CD8+ T cells through which it kills
virally infected cells. Thymosin alpha 1 has a negative effect on IL-1β and
tumor necrosis factor-α, which in turn leads to a decreased inflammatory
response and is quite beneficial in conditions such as chronic hepatitis and
acute pancreatitis.
Thymosin alpha 1 has exhibited
the ability to restrain tumor growth, hence its use in the treatment of various
cancers. It has anti-proliferative properties which have been exhibited in lung
and liver tumor metastases.
Since thymosin alpha 1 is a
polypeptide naturally present in the thymus, it plays a fundamental role in the
control of inflammation, immunity, and tolerance. Thymosin alpha 1 has an
immune-modulating action through its interaction with toll-like receptors. Due
to the action of thymosin alpha 1 on other cell types, it is used as a
therapeutic agent for diseases with evident immune dysfunction. Clinical trials
with thymosin alpha 1 for diseases like DiGeorge syndrome, non-small cell lung
cancer, hepatocellular carcinoma, hepatitis B and C, HIV, and melanoma have
been conducted and yielded promising results. FDA approved the orphan drug
thymalfasin (Zadaxin) for treatment of malignant melanoma, chronic active
hepatitis B, DiGeorge anomaly with immune defects, and hepatocellular carcinoma
due to its immunomodulatory and anti-tumor effect.
Thymosin
alpha 1 for auto-immune autism flare-ups?
Thymosin alpha 1 is no
wonder drug for autism, but it looks like it has a place in the autism toolbox,
for when symptoms take a sharp turn for the worse and you need a reset back to
your baseline autism.
If it solves the flare-up, great. If not, you just move on to the next option.
Conclusion
Italy does seem to have a different view of medicine. They are big on the medical use of probiotic
bacteria. They have treatments for GI problems that seem to be unheard of in
other countries. It is home to the novel idea, that I found appealing, to use
nerve growth factor (NGF) eyedrops to prevent dementia.
Italy is also home to the use of Thymosin alpha 1 shots, to reset
the immune system after an immune-related autism flare-up. I think it is a great idea and I doubt it is
expensive.
Most readers of this blog
are in North America, where Thymosin alpha 1 is not an approved drug. In China,
India, Italy and another 30 countries it is widely available.
As Zadaxin, Thymosin alpha 1, is produced by SciClone Pharmaceuticals in China. They provide the following summary:
http://www.shijiebiaopin.net/upload/product/2011121219115812.PDF
It looks like our readers who have an autism doctor in Italy have some interesting options.
Wayne State University never sought patent protection for Thymosin alpha 1 in
China, which they now regret.