Today’s post returns to folate deficiency, but before that a quick mention of magnetic/electrical brain stimulation therapies for autism without impaired cognition.
I encountered a new term IC-ASD. It
stands for intellectually capable autism spectrum disorder. Most people with
autism these days seem to have IC-ASD. Some struggle and some do not.
Objective
This
study aims to evaluate the efficacy of repetitive transcranial magnetic
stimulation (rTMS) and transcranial direct current stimulation (tDCS) on
repetitive/stereotypical behaviors and cognitive/executive functions in
children and young adults with intellectually capable autism spectrum disorder
(IC-ASD).
Methods
Literature
searches across PubMed, Web of Science, Cochrane Library, Embase, and Scopus
were performed to identify randomized controlled trials (RCTs) evaluating the
efficacy of rTMS and tDCS in children and young adults with IC-ASD. The search
encompassed articles published up to April 25, 2025. The standardized mean
difference (SMD) with 95 % confidence intervals (CI) was calculated and pooled.
Sensitivity and subgroup analyses were conducted to assess potential sources of
heterogeneity and refine the robustness of the findings.
Results
This meta-analysis included 18 RCTs
involving 813 participants. Compared with sham interventions, tDCS demonstrated
significant improvements in social communication, repetitive and stereotypical
behaviors, cognitive and executive functions among individuals with IC-ASD (e.g., Social Responsiveness Scale: SMD =
–0.48; 95 % CI: –0.75 to –0.22; p < 0.01). Similarly, rTMS improved social
communication, repetitive and abnormal behaviors (Social Responsiveness Scale:
SMD = –0.21; 95 % CI: –0.42 to –0.00; p < 0.05; Repetitive Behavior
Scale-Revised: SMD = –0.62; 95 % CI: –1.17 to –0.07; p = 0.04; Aberrant
Behavior Checklist: SMD = –0.53; 95 % CI: –0.79 to –0.26; p < 0.01). No
significant heterogeneity was observed across studies.
Conclusion
tDCS and rTMS may enhance cognitive and
executive functions and reduce repetitive behaviors in children and young
adults with IC-ASD. However, these
findings require careful interpretation due to the limited high-quality studies
and variability in treatment protocols. Future research should prioritize the
development of standardized protocols to address inconsistencies in stimulation
parameters (including frequency, intensity, and duration) and core outcome
sets. Additionally, larger-scale, rigorously blinded multi-center RCTs are
necessary to accurately evaluate the clinical efficacy and applicability of
these neuromodulation techniques in these populations.
rTMS and tDCS look like interesting
non-pharmaceutical options for those with milder types of autism. How well they
work in those with lower cognitive function is not addressed.
Back to Folate
Deficiency
Stephen recently highlighted a Chinese
study that looked at the relevance of mutations in the genes MTHFR, MTR, and
MTRR to try and identify those most at risk of folate deficiency.
I also highlight research into
treating some of the downstream consequences that occur when folate metabolism
is impaired. The lack of folate disrupts the immune system causing anomalies
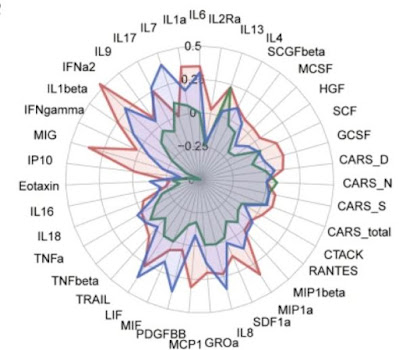
such as low NK cells, low NKT cells, high TNF-alpha.
Immunodeficiency
(Low NK and NKT cells): The
deficiency in these crucial innate immune cells means the body's ability to
fight off infections (particularly opportunistic ones) and perform immune
surveillance (e.g., against abnormal cells) is compromised. This
immunosuppression is a direct consequence of the impaired cell proliferation
due to the folate cycle defect.
Systemic
Inflammation (High TNF-alpha):
Despite the low numbers of certain immune cells, there can be an overproduction
of pro-inflammatory cytokines like TNF-alpha. This leads to chronic systemic
inflammation. This phenomenon is often referred to as hypercytokinemia.
Beyond TNF-alpha, you might expect a
possible overproduction of:
- Interleukin-1 beta (IL-1β): This is a potent pro-inflammatory
cytokine involved in various immune responses and neuroinflammation.
- Interleukin-6 (IL-6): Another major pro-inflammatory cytokine
that plays a role in systemic inflammation and can affect brain
development and function.
- Interferon-gamma (IFN-γ): This is a key cytokine in Th1 immune
responses and is also pro-inflammatory.
The recent Chinese study concludes
that high-dose folinic acid appears to be a promising intervention for children
with autism. Its efficacy is notably associated with specific folate metabolism
gene polymorphisms. The researchers suggest that high-dose folinic acid may
help to improve neurodevelopmental outcomes by alleviating the folate
metabolism abnormalities caused by single or combined mutations in these genes.
This research indicates that providing
a metabolically active form of folate (folinic acid, calcium folinate,
leucovorin etc) can be a direct approach to address the underlying metabolic
challenges in a subset of people with autism who have specific genetic
predispositions related to folate metabolism. Children with MTHFR A1298C or
MTRR A66G mutations showed greater improvements in various developmental
domains compared to those with the standard versions.
The intervention group demonstrated
significantly greater improvements in social reciprocity compared to the
control group.
No significant adverse effects were
observed during the intervention period.
How does this fit
in with US research into brain folate deficiency in autism
US researchers consider an autoimmune
mechanism where the body produces antibodies that specifically target the
Folate Receptor Alpha (FRα). FRα is a crucial protein responsible for
transporting folate across the blood-brain barrier (and into other cells).
When these antibodies bind to FRα,
they block or interfere with the normal transport of folate into the cells,
particularly into the brain. This results in Cerebral Folate Deficiency (CFD),
where folate levels in the cerebrospinal fluid are low, despite potentially
normal folate levels in the blood.
US research indicates that FRAAs are
prevalent in a significant percentage of children with ASD (up to 70% in some
studies) and are associated with specific physiological and behavioral
characteristics.
Treatment with folinic acid/
leucovorin has been shown to be effective in many children with autism who are
positive for FRAAs, improving symptoms like communication, irritability, and
stereotypical behaviors. It is believed that high doses of folinic acid can
overcome the transport blockade caused by the antibodies
The US and Chinese research avenues
complement each other by identifying different, but potentially converging,
pathways that lead to folate dysfunction in autism, both of which demonstrate
the therapeutic potential of folinic acid.
Here is the Chinese paper:
Safety
and Efficacy of High-Dose Folinic Acid in Children with Autism: The Impact of
Folate Metabolism Gene Polymorphisms
Background/Objectives: Research on the safety and efficacy of
high-dose folinic acid in Chinese children with autism spectrum disorder (ASD)
is limited, and the impact of folate metabolism gene polymorphisms on its
efficacy remains unclear. This trial aimed to evaluate the safety and efficacy
of high-dose folinic acid intervention in Chinese children with ASD and explore
the association between folate metabolism gene polymorphisms and
efficacy. Methods: A 12-week randomized clinical trial was
conducted, including 80 eligible children with ASD, randomly assigned to an
intervention group (n = 50) or a control group (n =
30). The intervention group was administered folinic acid (2 mg/kg/day, max 50
mg/day) in two divided doses. Efficacy was measured using the
Psycho-Educational Profile, Third Edition (PEP-3) at baseline and 12 weeks by
two trained professionals blind to the group assignments.
Methylenetetrahydrofolate reductase (MTHFR C677T, MTHFR A1298C),
methionine synthase (MTR A2756G), and methionine synthase reductase
(MTRR A66G) were genotyped by the gold standard methods in the
intervention group. Results: 49 participants in the
intervention group and 27 in the control group completed this trial. Both
groups showed improvements from baseline to 12 weeks across most outcome
measures. The intervention group demonstrated significantly greater
improvements in social reciprocity compared to the control group. Children
with MTHFR A1298C or MTRR A66G mutations
demonstrated greater improvements in various developmental domains than wild
type. Folinic acid may be more effective in certain genotype combinations, such
as MTHFR C677T and A1298C. No significant adverse effects were
observed during the intervention. Conclusions: High-dose
folinic acid may be a promising intervention for children with ASD, and its
efficacy is associated with folate metabolism gene polymorphisms. High-dose
folinic acid intervention may promote better neurodevelopmental outcomes by
alleviating folate metabolism abnormalities caused by single or combined
mutations in folate metabolism genes.
Treating the
downstream consequences of low brain folate
Today’s next papers highlight Infliximab,
IVIG, Propes, and Inflamafertin as immunomodulatory therapies that target the
downstream consequences of folate deficiency; they do not address or improve
the underlying lack of folate.
Folate Deficiency
in the Brain: This means there
is an inherent problem in the body's ability to process or utilize folate, even
if dietary intake is sufficient. It is often due to mutations in genes encoding
enzymes of the folate cycle (like MTHFR) or transporters. This leads to issues
with DNA synthesis, cell proliferation, and methylation, impacting various
systems, including the immune system.
Infliximab
Infliximab is a TNF-alpha inhibitor.
It blocks the activity of TNF-alpha, a key pro-inflammatory cytokine.
It does not put more folate into the
system or fix how folate is metabolized. It is like putting out a fire
(inflammation) that was started because of a broken electrical wire (folate
deficiency's impact on immunity).
IVIG (Intravenous
Immunoglobulin)
IVIG is a broad-acting
immunomodulatory therapy composed of pooled antibodies from thousands of
healthy donors. Its mechanisms are complex and include neutralizing
autoantibodies, blocking Fc receptors, modulating cytokine production,
affecting T and B cell function, and influencing complement activation.
IVIG aims to rebalance a dysregulated
immune system, reduce inflammation, and sometimes provide passive immunity. It
is like resetting an overactive or misdirected immune alarm system. The effect
may not last.
Propes
Propes contains alpha- and
beta-defensins and has a "pronounced immunoactivating and
lymphoproliferative effect." It directly stimulates the growth and
activity of immune cells like NK and NKT cells. It directly addresses the numbers
and activity of NK and NKT cells that are deficient due to the folate cycle
problem. It makes the existing cells (or promotes the creation of new ones)
work better, despite the underlying folate issue.
Inflamafertin
This drug, containing alarmines and
adrenomedulin of placental origin, has "pronounced anti-inflammatory and
immunomodulatory effects mediated by the induction of interleukin 10
synthesis." Its role is to temper the immune activation and ensure a more balanced, anti-inflammatory
environment.
In summary
These therapies are all symptomatic or
compensatory treatments for the consequences of genetic folate deficiency on
the immune system and the body. They address the resulting immunodeficiency,
inflammation, and associated clinical symptoms (like behavioral issues or
opportunistic infections).
They do not:
- Add more folate to the body (like folic
acid or L-methylfolate supplementation would).
- Correct the genetic defect that causes
the folate cycle deficiency.
- Improve the body's intrinsic ability to
metabolize folate.
Genetic deficiency in the folate cycle disrupts fundamental cellular processes required for the normal development, proliferation, and function of NK and NKT cells, leading to their deficiency in affected children. This deficiency, in turn, contributes to the complex immune dysregulation often seen in autism.
Key Findings on
NK Cells:
- Initial Deficiency: A significant number of children in the
study group (53 patients) had an initial deficiency of NK cells.
- Response to Immunotherapy:
- During the 3-month course of Propes and
Inflamafertin, the average number of NK cells in the blood almost doubled.
- NK cell counts reached the lower limit
of normal in 74% (39 out of 53) of the patients with a deficiency.
- There was a strong statistical link
between the immunotherapy and NK cell normalization.
- Sustainability: A notable finding was that the NK cell
numbers returned to almost their initial level within 2 months after the
immunotherapy was stopped. This suggests that the effect on NK cells might
be temporary and dependent on continuous treatment.
Key Findings on
NKT Cells:
- Initial Deficiency: A larger proportion of children in the
study group (87 patients) had an initial deficiency of NKT cells.
- Response to Immunotherapy:
- The average number of NKT cells in the
blood increased by half during the 3-month immunotherapy course.
- NKT cell counts were normalized in 89%
(78 out of 87) of the patients with a deficiency.
- There was an even stronger statistical
link between the immunotherapy and NKT cell normalization compared to NK
cells.
- Sustainability: Importantly, the NKT cell numbers continued
to grow for an additional 2 months after the discontinuation of the
immunotropic drugs. This suggests a more sustained and potentially
longer-lasting effect on NKT cells.
Overall
Conclusions from the Study:
- Combination immunotherapy with Propes and
Inflamafertin is presented as an effective treatment strategy for the
immunodeficiency (specifically NK and NKT cell deficiency) found in
children with ASD linked to genetic folate deficiency.
- Both biological drugs were able to
normalize the reduced numbers of NK and NKT cells during the 3-month
treatment period.
- The study highlights that the effect on NKT
cells was more frequent, stronger, and more lasting compared to the effect
on NK lymphocytes.
The research papers:
In
SG, there was a pronounced positive dynamics in the direction of hyperactivity,
hyperexcitability and stereotyped behavior, but no significant effect was noted
on the stability of eye contact and the development of expressive-receptive
language, while in CG some positive changes were achieved specifically in terms
of expressive language and the level of eye contact, which indicates different
points of action of infliximab and specialized educational programs (Table
11.1). The psychotropic
effect obtained with infliximab differs from that of intravenous
immunoglobulin, which has also demonstrated clinical efficacy in ASD associated
with GDFC [10, 12]. The changes induced by infliximab are more pronounced
and develop in a shorter time frame, but they are significantly narrower in
terms of the spectrum of positive psychotropic effects compared to high-dose
immunoglobulin therapy, which has a total modifying effect on the psyche of
such children.
Materials and methods. This prospective controlled single-center non-randomized clinical study included 225 children diagnosed with autism spectrum disorders associated with genetic deficiency of the folate cycle. The diagnosis of autism spectrum disorders was made by psychiatrists from regional hospitals or specialized departments according to DSM–IV–TR (Diagnostic and Statistical Manual of mental disorders) and ICD–10 criteria. Children were recruited into the study group (SG) in 2019–2020. These were patients from different regions of Ukraine aged 2 to 9 years, in whom elevated serum TNF-alpha concentrations were observed. As is known, the phenotype of genetic deficiency of the folate cycle includes 5 main syndromes: autism spectrum disorders, intestinal syndrome (persistent enteritis/colitis) [7], PANDAS [4, 9], epileptic syndrome [5] and signs of pyramidal tract damage.
Conclusions.
Infliximab leads to significant improvements in hyperactivity and
hyperexcitability, as well as stereotypic behavior in children with autism
spectrum disorders associated with genetic deficiency of the folate cycle.
Responders to immunotherapy are 76 % of patients with this pathology, which is twice as high as with standard
therapy. However, there is no effect of infliximab on such manifestations of
autism as the level of eye contact and language development. Psychotropic
effects of infliximab immunotherapy are closely related to the normalization of
previously elevated serum TNF-alpha concentrations and are probably due to the
elimination of the pathological activating effect of this pro-inflammatory
cytokine on CNS neurons. In parallel, there is an improvement in other clinical
syndromes of genetic deficiency of the folate cycle in children with autism
spectrum disorders – intestinal pathology, epileptic syndrome, and PANDAS,
in the pathogenesis of which, as is known, TNF-alpha and the systemic and
intracerebral inflammation induced by this cytokine are involved. However,
under the influence of immunotherapy, there is no change in the dynamics of
motor deficit in children with symptoms of pyramidal tract damage. Further
clinical studies in this direction with a larger number of participants and
randomization are necessary to obtain more convincing data.
The
results obtained in this controlled non-randomized clinical trial indicate that
combination immunotherapy with Propes and Inflamafertin is an effective
treatment strategy for immunodeficiency caused by genetic folate deficiency in
children with autism spectrum disorders. These biological immunotropic drugs
are able to normalize the previously reduced number of NK and NKT cells in the
blood in this category of patients during a 3-month course of immunotherapy,
with a more frequent, stronger and more lasting effect on NKT cells compared to
NK lymphocytes.
Conclusion
Folinic acid supplementation is an
effective therapy for many people with autism. There are many anomalies that
appear, for example those people who test positive for the folate transporter
antibodies but a lumbar punction then finds normal levels of folate in the
brain. Many people report agitation or
aggression when children take calcium folinate at high doses, but this does not
seem to get noted in clinical trials. Nonetheless it looks like everyone with autism should at least make a trial.
Note that you should always add a vitamin B12 supplement when giving high dose calcium folinate. This is because more B12 will be required by the biological processes ongoing in the brain and deficiency will cause side effects.
Many people who respond well to
calcium folinate end up needing some kind of immunotherapy on top. IVIG is
extremely expensive and quite a bother if you need to take it forever. Some of the
therapies from the two papers today also involve a very large number of injections,
so are not really practical. The less intrusive immunotherapies look more practical but are not cheap.
I think that rTMS and tDCS will be attractive to those seeking non-pharmaceutical options that have a scientific basis. The same applies to low level laser therapy, also known as photobiomodulation therapy.